CANCER OF UNKNOWN PRIMARY FOUNDATION
Hospital diagnosis
Every hospital trust in England, Wales and Northern Ireland should have a MUO/CUP assessment service. (Scotland does not fall under the NICE CUP Guideline but has very similar processes.) The NHS standard target interval between urgent GP referral and first hospital appointment is 2 weeks throughout the UK. But many CUP patients will present as acutely ill, via emergency services, without seeing their GP first, and become recognised as a case of metastatic Malignancy of Undefined primary Origin (MUO).
If you have MUO, or suspected CUP, in you should be seen by the hospital MUO/CUP Team. In theory, the core of the hospital CUP multidisciplinary team (MDT) in England, Wales and N. Ireland includes:
- A named consultant oncologist
- A named consultant in palliative medicine
- A named cancer nurse specialist (CNS)
The hospital staff you are likely to see initially will be the oncologist of the CUP team and the CNS. They will be able to involve imaging and other specialists to consider each patient’s case in detail. The CNS is particularly important for patients. Patients should meet their local CUP clinical nurse specialist (CNS) within two weeks of referral (within one working day for inpatients) and be supported through investigation and treatment by the CUP CNS.
In patients of poor performance status, where further investigation is not appropriate, early referral to palliative care should be made.
This is the theory following the NICE Guideline and the Peer Review Measures which assess a hospital trust’s performance. However, not all hospitals are fully compliant, with a fully functioning CUP Team. If you want to see how different hospitals in England and Wales were rated for their CUP services in the external peer review exercise of 2016 you will find the report here.
The NHS NICE Clinical Guideline on CUP (CG104, July 10) gives clinicians carefully constructed, evidence-based, approaches to different CUP presentations. It classifies CUP into 3 stages:
- Malignancy of undefined primary origin (MUO). Metastatic malignancy identified on the basis of a limited number of tests, without an obvious primary site, before comprehensive investigation.
- Provisional carcinoma of unknown primary (provisional CUP). Metastatic (epithelial or neuro-endocrine) malignancy, identified on the basis of histology/cytology, with no primary site detected despite a selected initial screen of investigations, before specialist review and possible further specialized investigations.
- Confirmed carcinoma of unknown primary (confirmed CUP). Metastatic epithelial or neuroendocrine malignancy identified on the basis of final histology, with no primary site detected despite a selected initial screen of investigations, specialist review, and further specialized investigations as appropriate.
What the doctors will be trying to do with a patient that presents with MUO is to obtain sufficient clues to direct the patient to a site specific multi-disciplinary team (e.g. the breast or lung MDT) for treatment. Assuming the patient responds to treatment for that condition, he or she is no longer an MUO or CUP patient.
Identification makes diagnosis the key to effective treatment. The better the diagnosis, the better the chances of effective therapy leading to remission or substantial palliative benefit.
If further tests are required because the primary site remains undetected then the patient falls into the ‘provisional’ and then the ‘confirmed’ category. This is the pattern for a reasonably fit patient. For an elderly or very sick patient, perhaps suffering with other serious problems, it may be inappropriate to carry out some or all of the tests.
A bit more detail on processes for referral and management
As a patient you may not want more detail at this stage but your GP may. The cancer network that covers your hospital will have ‘local protocols’ that expand the NICE Guideline with more detail appropriate to the way they work and the different routes to diagnosis. For example the Thames Valley Cancer Network require the following:
Out-patients
If a GP has requested a CT scan or other imaging which shows suspected MUO, the patient should be referred to the CUP clinic under the 2-week wait system and be assessed face to face by a member of the CUP team within 2 weeks of the working diagnosis of MUO being made. The patient may be seen in a site-specific clinic if the clinical details indicate a likely primary or treatable syndrome. A&E should follow the same 2-week wait referral pathway as GPs for patients who are not being admitted to hospital.
In-patients
All hospital teams with an MUO in-patient should contact the local CUP team for review within one working day of the working diagnosis of MUO being made. (In many hospitals, the CUP and Acute Oncology Service (AOS) will be led by the same people). If the patient is to be discharged pending further investigations, the CUP team should arrange out-patient follow-up. These patients should remain under the care of the CUP team unless their care is referred to a site-specific team or to palliative care. Whilst an in-patient, the CUP team will advise on the appropriate investigations and review the patient, but the overall care of the patient may be under another team, depending on the local arrangements in each hospital. In patients of poor performance status, where further investigation is not appropriate, early referral to palliative care should be made.
Investigations
Responsibility for the in-patient investigations will fall to the admitting or ward team under the guidance of the AOS/CUP team. Responsibility for the outpatient investigations will lie with the CUP team if the patient has been referred to the CUP team. If the primary site is found on subsequent investigations, the patient’s care will then be referred to the site-specific team, or if the patient has a specific treatable syndrome within CUP. The patient will need to be referred on from the CUP team to the site-specific team in this instance.
MDT discussion
All patients with MUO/provisional CUP should be discussed at the next CUP MDT
meeting for :
• Advice on remaining investigations needed to confirm the diagnosis of CUP or establishment of a primary site
• Any necessary decision regarding suitability for ‘active treatment’ (chemotherapy, radiotherapy, biological therapy or surgery)
• Treatment planning decisions.
Any site-specific MDT, on being referred any MUO patients, should refer them on for discussion by the CUP MDT. The CUP MDT may also seek advice on a CUP patient from a site-specific MDT depending on the particular features of the case.
What sort of investigations is the patient likely to have?
The investigations should be directed by the NICE Guideline for CUP. The sort of investigations, at different stages may include: medical history, a complete physical examination, tumour biopsy (a sample of tissue taken for examination – see below), chest X-rays, blood cell analysis, urine and stool analysis, radiographic imaging using scans such as CT. See Tests you may have for further information and also the patient-friendly Macmillan Cancer Support booklet on Understanding CUP (2019) .
Why so many tests? Some tests are more likely to reveal particular cancers and the oncologist will also want to use different sources to gather as much evidence as possible about the origin of the cancer for treatment. The oncologist will not be working alone – he or she will be gathering information from a team of experts in different fields. This is particularly the case with CUP where the cancer cells may be ‘poorly differentiated’. It may help you to think of this as being like a crime scene. The oncologist, like the detective, will be calling-in the different agencies – like the fingerprint expert or in this case the pathologist – and gathering and evaluating all the evidence trying to prove various parts of your anatomy guilty or innocent.
Each tumour is unique and each patient is unique.
The biopsy
The overall purpose of the biopsy is to get a better diagnosis and therefore a better prediction of the outcome and treatment benefit. This is done by the pathologist comparing the tumour tissue with normal tissue. Of all the investigations the key one in identifying the primary is likely to be the biopsy. A biopsy (which may not be appropriate for someone who is very sick) is usually performed as an outpatient procedure. However, some biopsies – such as biopsy of an internal organ – require a general anaesthetic and an overnight stay in hospital.
The cancer specialist will decide which type of biopsy is best and the sample of tissue will be analysed by a pathologist using a microscope and chemical tests. For most CUP patients a Core or Incisional biopsy is necessary:
- Punch Biopsy. This is where, for example with possible skin cancer, the doctor very simply removes a small piece of skin with an instrument that looks like a tiny apple corer
- Fine-Needle Aspiration (FNA). Multiple samples of tissue or fluid are removed through a small bore needle guided into the cancerous tissue. This is more likely to be used to help determine whether a patient has cancer rather than for determining the primary site.
- Core Needle Biopsy. A larger bore needle is used allowing a more generous specimen and therefore a more accurate diagnosis.
- Incisional Biopsy. A small wedge of tissue is removed providing a good sample for examination. Excisional Biopsy. This is when an entire suspect area is removed.
Using the biopsy to make the diagnosis
Looking at the biopsy and/or blood samples, and if the lesion is malignant, the scientists (pathologists) will separate CUP into categories and try to increase their focus with further subtypes, if possible.
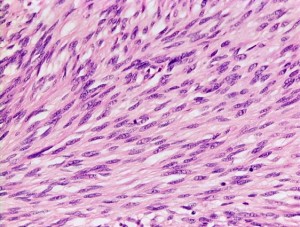
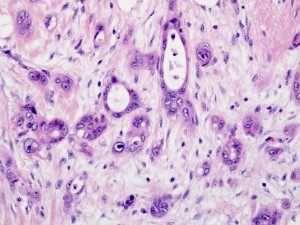
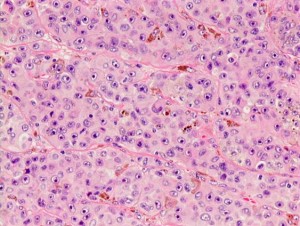
The top level of classification is the broad type of cancer and this is determined by looking at the patient’s tumour cells under the microscope . The images below give some idea of what the pathologist is looking at, at the top level, and the malignant cells will look very different:
Carcinoma
Melanoma
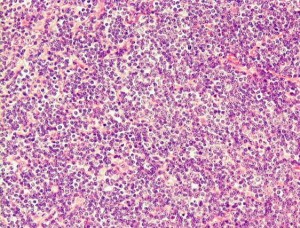
Lymphoma
This is where the language gets complicated but it is worth at least knowing the names of the categories below as they may be used by oncologist to give you a CUP diagnosis. So, looking under the microscope, and using stains, the pathologist will see images such as the ones above; and, if carcinoma, he or she will then try and identify a subtype such as squamous, neuroendocrine, or adenocarcinoma. If, through further tests, the pathologist identifies adenocarcinoma, then he or she will try see whether the primary site e.g. prostate, lung, breast, colon, ovary, pancreas, biliary tract or stomach, can be predicted from the visible evidence.
The majority of CUP are adenocarcinomas or undifferentiated tumors; less commonly, squamous cell carcinoma, melanoma, sarcoma and neuroendocrine tumors can also present with a primary site of origin that cannot be determined.’ (Source: National Cancer Institute – USA).
Usually, the metastatic (cancer-spread) distribution helps the oncolgist and pathologist to establish the type of cancer because certain secondaries (secondary sites of the cancer) tend to come from certain primaries (primary sites of the cancer). But because CUP is ‘atypical’ in its spread – in other words, it doesn’t follow the norms of cancer spread – the location of the secondaries may not be particularly helpful in identifying a primary site.
The pathologist will provide the oncologist with a further sub classification. The categories below are ranked by probability (that is to say Adenocarcinoma is the most common for CUP patients):
- Adenocarcinoma – a form of cancer that can arise in most internal organs. It is difficult for the pathologist to determine accurately the site of origin from a metastatic sample. (Carcinoma is any cancer that arises from epithelial cells – a tissue composed of a layer of cells that originates in glandular tissue. Epithelium is one of four primary body tissues.)
- Poorly differentiated cancer. A cancer that is very poorly differentiated is called anaplastic. Anaplasia is a term that refers to the histologic grade of a tumor. Anaplastic tumors are poorly differentiated, meaning that their cells do not resemble normal cells. Some very treatable cancers may be diagnosed initiallyas poorly differentiated. (Grade is a marker of how differentiated a cell is. Grade is rated numerically -1 to 4 or descriptively – e.g., ‘high grade’ or ‘low grade’. The higher the numeric grade, the more ‘poorly differentiated’ or ‘high grade’).
- Squamous cell cancer. This is a form of cancer of the carcinoma type (a malignant tumour of epithelium) that may occur in many different organs, including the skin, mouth, esophagus, lungs, and cervix. Many of these cancers can be treated successfully.
- Neuroendocrine carcinoma. The rarest category for CUP. Neuroendocrine tumours (NETs) are tumours composed of neuroendocrine cells, which are cells that produce and secrete regulatory hormones and are present in the nervous and endocrine/hormonal systems throughout the body. Small cell carcinoma, when not in the lung, is thought to originate from neuroendocrine cells, which are found in the epithelium.
- Undifferentiated neoplasms (tumours). Sometimes it’s not possible to determine which of the above categories it is and further tests may be needed.
If no primary site is identified by the tests the oncologist uses the categories above to supplement all the information available to him or her to judge the best treatment. This may be ’empiric chemotherapy’; that is to say, chemotherapy based on previous experience of patients presenting with similar characteristics. Molecular Profiling (not routinely funded by the NHS) looking at the DNA of the tumour can augment the process explained above in order to understand better the likely primary characteristics or ‘actionable mutations’ of the cancer. Molecular profiling is explained in the section Tests you may have.